How I used diet & nutrition during my Long COVID recovery (pt. 1)
How unresolved inflammation is a key driver in Long COVID, how that relates to diet, and what you can do about it. Plus, a helpful handout by the Long COVID clinic at UCSF (thanks!)
I’m not a doctor, nor a scientist, and the following is not intended as medical advice. I’m just one person who has (mostly) recovered from a severe version of Long COVID and has done a ton of research, sharing my experience and learnings. Please always listen to your body, and always ask your medical providers what’s right for you (in particular when starting a new protocol, such as making major changes to your diet).
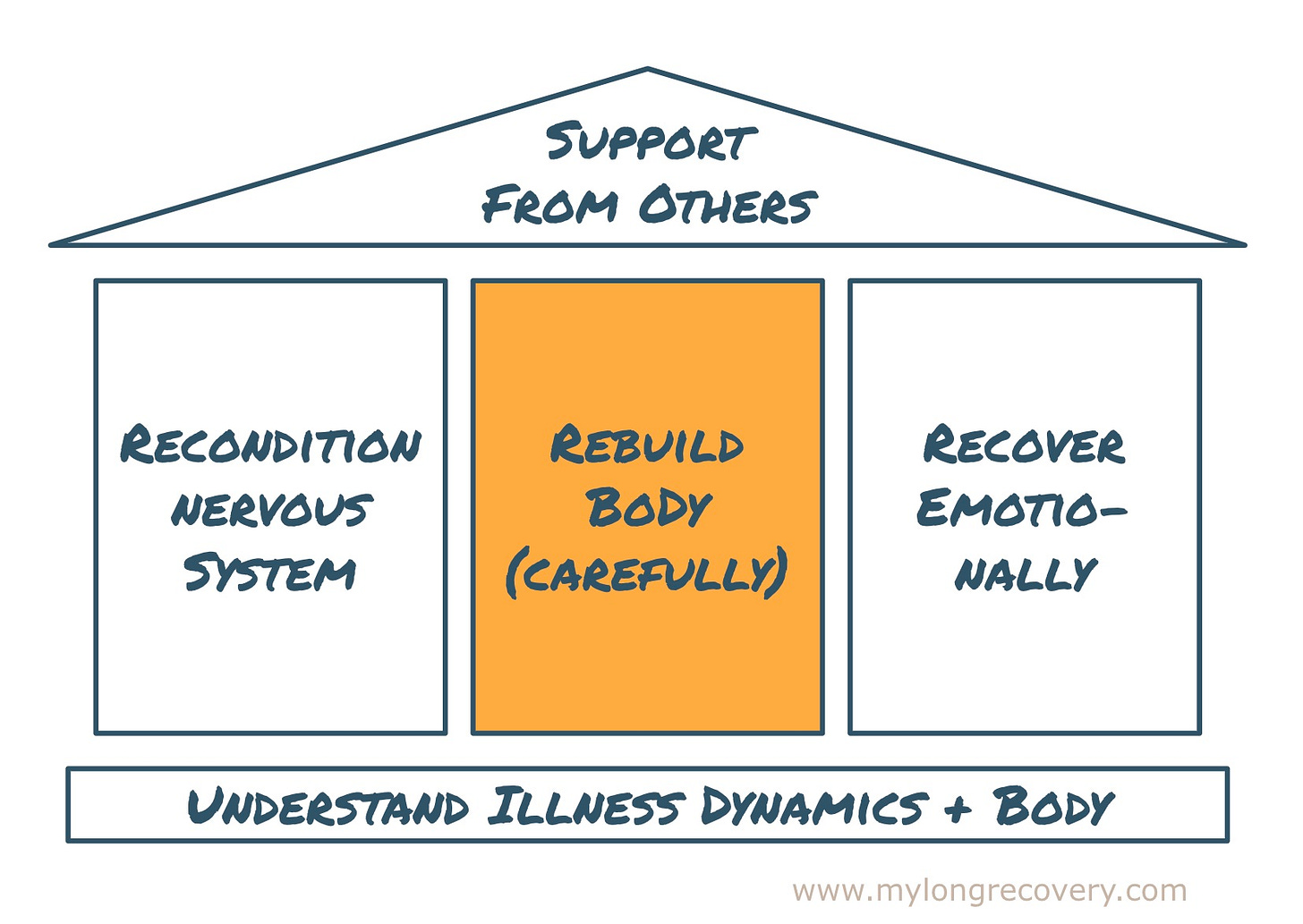
In my recovery framework, today’s post on inflammation and diet during Long COVID is part of the pillar physical recovery tools, or “rebuilding the body”. Here’s how it fits in:
A lot has been written on diet and nutrition, and what you eat is obviously a super personal decision. This is even more the case if you’re dealing with chronic illness. I personally learned a lot on diet and nutrition during my recovery, and it’s caused fundamental changes in what I (want to) eat. So I’m sharing what I learned, and you can take the bits from it that feel relevant to your own journey.
I’ll split this up into two posts, the first one today is about the theory - why diet is relevant to Long COVID recovery, and how inflammation plays a role in the illness. The second post in the next weeks will be the practical part, i.e. how I adjusted my diet during recovery. I’ll share what changes I actually made, what made those changes easier, and the mistakes I’d avoid if I’d do it again.
How I learned about nutrition and Long COVID
I always thought I had a pretty healthy diet - it was part of my lifestyle, like for most of the people in my fit & active circles. So when I first started reading about diet, inflammation, and Long COVID, I was surprised that not everything I had assumed to be healthy food was actually good for me—let alone able to support recovery from severe, multi-systemic illness.
I wasn’t looking for information on diet or nutrition particularly - my symptoms didn’t seem food related in any way. I came across nutrition and diet by chance, reading Dr. Carla Kuon’s book on Long COVID recovery (I’ve linked to it previously, see here). Months into my illness and recovery, and after many medical dead ends, I was finally lucky to get into treatment with her at UCSF (for those not in the US - University of California, San Francisco, a leading teaching hospital). That treatment initially consisted of 3 group sessions, the first of which was entirely focused on diet. With Dr. Kuon’s permission, I am including the handout from that session here: UCSF handout on Long COVID, inflammation and diet. (Thank you Dr. Kuon for very generously letting me share this publicly!) I’ll be sharing the handouts of the other two sessions (one on supplements and nutrients, and one on stress physiology and exercise) in future posts.
Inflammation and Long COVID
So, why is diet is so important in Long COVID recovery? One of the key drivers for the persisting symptoms in Long COVID is inflammation in the body, per research by Akiko Iwasaki at Yale1.
The way Dr. Kuon at UCSF explained it, “COVID can kick off inflammatory pathways in the body to such high levels, the body is unable to resolve them without added help.”2 According to her, there are 5 drivers to inflammation in Long COVID:
Classic inflammation
Histamine-related inflammation
Autoimmune-related inflammation
GI (gastro-intestinal)-driven inflammation, and
Neuro inflammation
Patients can have one of these drivers, or several. This is why symptoms can vary so much between people with Long COVID, and why it’s hard to diagnose. Dr. Kuon explains each of these types of inflammation in great detail in her book, if you’re curious (I’ve linked to the book here).
She also writes that “Long-term inflammation can affect everything negatively from head to toe”.3 For example,
Brain —> cognitive dysfunction, memory loss
Circulatory system —> heart disease, stroke, blood clots
Immune system —> Lowered immunity, frequent viral infections
Etc.
This really clicked for me - it was the first explanation I heard that shed light on why I was experiencing such a broad range of serious and seemingly unconnected symptoms, and how even the most basic things in my body were not functioning properly anymore.
So why does that inflammation not just resolve, like after other infections? You know, when you might have a fever or other symptoms for a few days, and then get back to normal and move on with your life? The way I understand it now, COVID (and other viruses) can, if you’re unlucky, totally overwhelm the body. That overwhelm disturbs a range of processes in the body, and knocks them out of balance. These processes usually run in the background, as you go about your day—like turning food and oxygen into energy, repairing damaged cells, fighting off bacteria and viruses, removing toxins, hormone production, etc. Because they are all interconnected and interdependent, once they are knocked out of balance, the body can have a very hard time shifting back into equilibrium. We can support it however, by supplying the right nutrients, i.e., the building blocks for all the biochemical reactions that need to take place (see Dr. Kuon’s book for details, I found this all fascinating).
How to address inflammation during Long COVID recovery
The good news is that there are things we can do. We can supply these building blocks in higher quantities, directly addressing the excess of inflammation, and help the body shift back. According to Dr. Kuon, the main levers for reducing inflammation are (1) proper nutrition and anti-inflammatory diet, and (2) anti-inflammatory supplements (I’ll write about the supplements another time).
The first important thing is that a healthy diet is very individual - people have a wide range of food intolerances, for example. There is a common denominator, however. According to Dr. Kuon, this is “a plant-based diet rich in anti-inflammatory foods such as the omega-3 fats, rich in antioxidants, and which avoids pro-inflammatory foods”.4 She recommends this anti-inflammatory diet as the basis during Long COVID recovery (to be adapted if you have additional conditions or complications, like histamine intolerance).
Dr. Andrew Weil, who pioneered Integrative Medicine in the US, created the pyramid below as a summary of the anti-inflammatory diet, showing which foods should be eaten in roughly which ratio:

You can explore this in detail on Dr. Weil’s website.
Like most of you presumably, I had seen this pyramid many times before, and was generally eating healthily. But reading in detail how certain foods contribute to inflammation, and how inflammation is a huge driver for Long COVID, it hit very differently. I shifted from eating “generally healthily”, to implementing this diet very strictly.
I’ll stop here for today, and share next time what I actually changed (to me that pyramid above doesn’t really cut it, so I’ll share a list of actual things I ate more of and less of). I’ll also share what made that major diet change easier during an already very challenging time, and some major mistakes I made in the process (so you don’t have to ;)).

Let me know if you have specific questions, and I can try to answer them next time! Also, I’m curious what’s worked for you diet-wise during Long COVID?
Take good care of yourself,
Nicole
PS (unrelated topic): As I’ve mentioned before, breathwork has also been a really impactful tool in my recovery. Based on that experience, I’ve been training as a breathwork coach since March, expecting to graduate in November (will share more of my learnings here soon!). I’ll have 3 spots for 1:1 breathwork coaching available during this final phase of my training (at a reduced rate). A great opportunity if you’ve been wanting to explore breathwork as a recovery tool, or if you’re already using it and are looking for 1:1 support. Details here
Professor of Immunobiology at Yale, and one of the leading researchers on Long COVID globally
UCSF handout, see above
The LONG COVID Solution by Carla Kuon, MD (page 35)
The LONG COVID Solution by Carla Kuon, MD (page 44)





I'm sold now to read Dr Kuon's book! It was already so interesting to see the handout, because I was told to avoid histamine, but not to avoid lectins. I ended up avoiding them because I got symptoms whenever I ate them.
I was actually told to follow a specific diet to enhance mitochondrial metabolism. It's found here in case anyone wants to take a look at it (this is just the food list I was given): https://nowhealthpalmer.com/wp-content/uploads/2017/08/MitoFoodPlan_v5-1.pdf
The entire rationale behind it is here: https://centerforfunctionalmedicine.com/wp-content/uploads/2016/10/mito_food_plan_comprehensive_guide_v3.pdf
And here are some recipes: https://www.hamptonfamilypractice.com/wp-content/uploads/2018/03/Mito-Food-Plan.pdf
Very interesting article and the açaí bowle looks delicious. I'm curious if you will write about celery juice next week. It helped me a lot with my fatigue. 🥬✨️