Diet & Long COVID recovery, pt. 2: The actual changes I made
What I ate more of during recovery, and what I ate less of. And the reasons why
I’m not a doctor, nor a scientist, and the following is not intended as medical advice. I’m just one person who has (mostly) recovered from a severe version of Long COVID and has done a ton of research, sharing my experience and learnings. Please always listen to your body, and always ask your medical providers what’s right for you (in particular when starting a new protocol, such as making major changes to your diet).
One thing before I start: Thank you everyone who reached out about the “Breathwork for Long COVID Recovery” coaching program I mentioned last time. I’ve settled on dates, and it’ll run mid October to mid November (four weeks with one 1:1 session each). Right now, I have 2 spots left. Respond to this email or message me if you are interested, happy to answer any questions!
Secondly, those of you who read this regularly might have noticed—it’s been a minute! It’s been a really busy month for me. Job interviews, moving apartment, trying to furnish the new place (so far, failing - I’m still sleeping on an airbed a month later lol), planning the breathwork program, plus some required travel, all happening at the same time. I also ran my first workshop as a breath coach, at an event for startup founders & investors a couple of weeks ago, too, which was super fun. So, a lot going on! It was honestly pretty overwhelming. With all that happening and timing to large parts outside of my control, I made extra sure to continue to take good care of my body, which meant that I had to press pause on a few things (like writing the newsletter), and do others more slowly than I’d like (getting furniture, responding to messages - sorry everyone!). And I’ll make sure that the next few months are more restful again as I catch up. But it’s been an exciting month, and it feels awesome to be able to handle that kind of pace again when needed.
So much for my life update, on to nutrition.
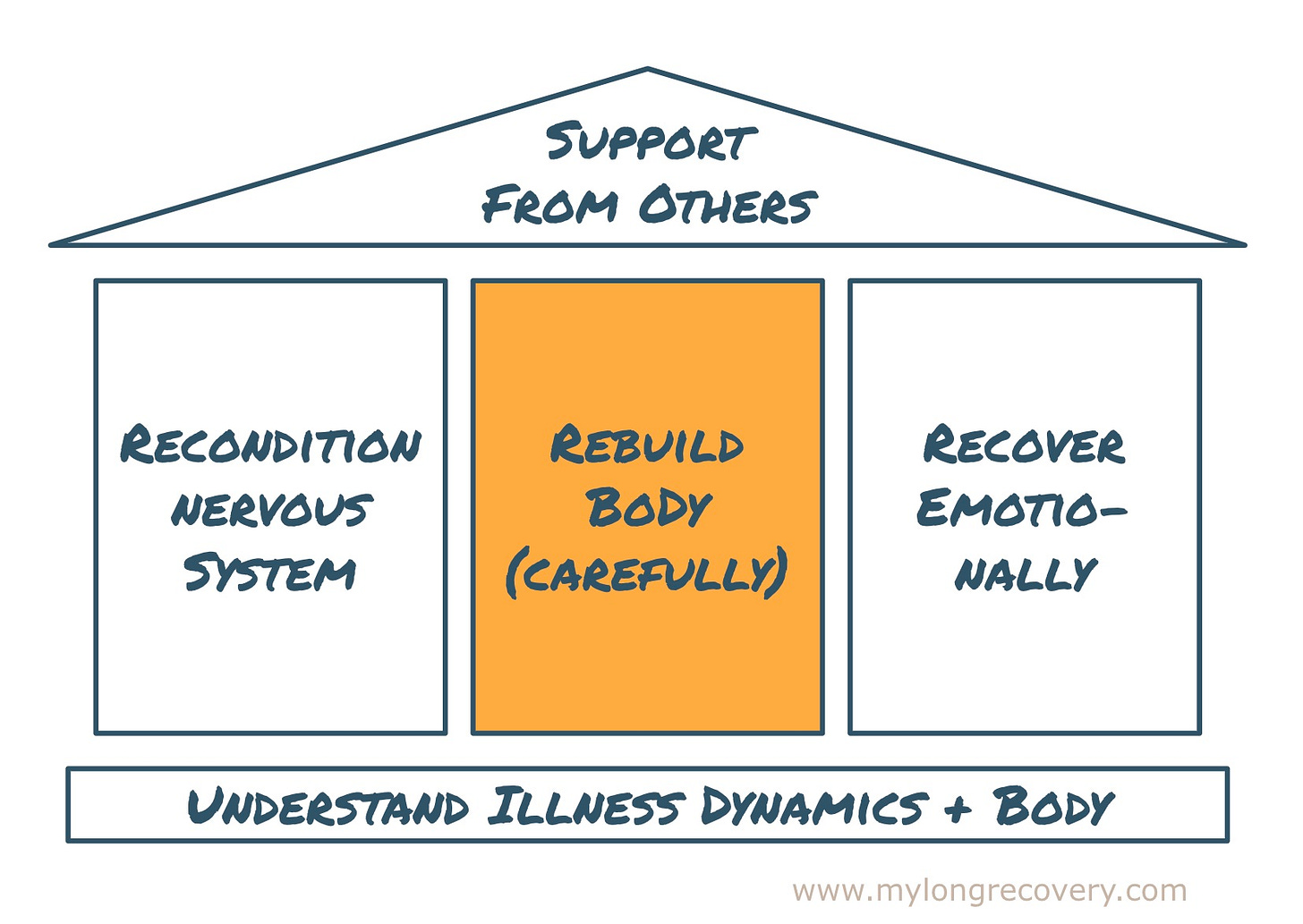
In my previous post on diet during recovery, I shared what I learned about inflammation and Long COVID, and the diet that the UCSF1 Long COVID clinic recommends to help tackle it. So now that we’ve established that bringing down inflammation is key, and that we can impact inflammation with our diet, what did that mean for me in practice? That is what this part 2 is about. If you’re new here (hi & welcome!), nutrition is part of the physical tools in my recovery framework.
The changes I made to my diet during recovery
Firstly - diet is very individual, every body is different. You’ll need to figure out what works for your specific body, so take this with a grain of salt - I’m sharing here what worked for my body. I also assume that if you’ve had Long COVID for a while, you might have already experimented with diet, and tried some of the same things—maybe they have helped, maybe not. It’s often hard to figure out what works, because it’s so tricky to isolate the changes we make, and nutrition changes take a while to work (inflammation needs time to resolve). That’s why it’s important to know why certain foods can impact our health positively or negatively, and under what circumstances. It’s an ongoing journey of research for me. I suggest if you’re new to this, then start with my last post, which goes into the why. Today’s post is on the what.
So here is how I adjusted my diet, practically - my protocol. In summary, I went on a very strict anti-inflammatory diet, with some tweaks relevant to my specific body. This was primarily based on Dr. Kuon’s2 advice - as shared last time, but I found other sources too, once I had understood they key ways I needed to support my body.
What I ate more of
There are explanations to why each of these are important in reducing inflammation and promoting cell healing, so let me know in the comments if you have questions - I’ll focus on the “what” today, not the “why”.
Incorporating more whole grains, vegetables and legumes (this has been the foundation of my recovery diet)
Increasing my fish consumption, trying to eat it most days - in particular, omega-3 rich ones (e.g., salmon, black cod, anchovies)
Incorporating “superfoods” like blueberries, chia seeds, shiitake mushrooms and turmeric, which have a lot of antioxidants and anti-inflammatory agents (I used to think that “superfoods” were mostly marketing, but changed my mind after learning more)
Switching to all organic fruit and vegetables (I know this is cost prohibitive for many people - check the UCSF handout in my last post for the “dirty dozen”, the produce types for which it’s most crucial to go organic, due to the high rate of environmental toxins in the conventional version)
Drinking sufficient water, like 1.5-2L / day. I always find this hard but I paid extra attention to it during recovery, and everyone around made sure I was drinking my water, too. Hydration is always important, but crucial during recovery (biochemical processes like cell repair, clearing toxins etc. require fluids to function properly).
Incorporating more (healthy) protein - as someone who doesn’t eat a lot of meat, I did not have nearly enough protein in my diet at that point (might be different for you!).3 Protein is important in cell healing, and given the cell damage that the virus had caused in my body, I needed to provide my body the building blocks to repair itself. This meant a lot of fish and tofu, legumes, nuts and seeds like chia, quinoa, hemp seeds etc. A LOT more than what I was used to.
So far, so good. That was the fun part, unfortunately.
What I cut out
There are also a lot of things I cut out. During the worst months, I was 100% strict about this, which was rough. I love chocolate and various comfort foods, and it felt like the illness had already taken so much from me - the joy of eating was one of the last things I had left. What helped me do it was to see the restrictions as temporary (more on that next time), and to stay focused on the much bigger goal - getting my health back. In comparison, cutting out almost anything for a few months felt like a very small price to pay.
No caffeine. This one might be counter intuitive if you’re fatigued, but cutting out caffeine is crucial to our nervous system normalizing, which in turn, is key to our body’s ability to heal. I’ll write about the nervous system another time (I keep saying that! lol. I promise), but in short - you want to avoid anything that activates your sympathetic nervous system. Caffeine does that, unfortunately, so it’s important to avoid it while you recover.
No refined sugar. Same re nervous system—sugar is also activating. In addition, it’s generally bad for our health - so I tried to not burden my body even more, while it was struggling to heal.
No alcohol. Same re nervous system, plus it’s quite literally toxic to the body (don’t get me wrong, I’m a fan of a drink in general, but when the body is struggling so much already, it is not the right time).
No highly processed foods. The body needs nutrients. Highly processed foods don’t have as many of those. In addition, these foods contain a whole lot of harmful ingredients - additives, chemicals, unhealthy kinds of fat, sugar—that your body might struggle to process in its current state.
Very little meat. This one was relatively easy for me since I wasn’t eating much meat before anyway. During recovery I made a couple more changes—I ate no processed meat at all (see above), and if I did eat meat, it was poultry. Meat has been shown to be inflammatory (in particular, red meat).
No gluten. Gluten is inflammatory for many people. This was maybe the hardest, as I had a pretty pasta-heavy diet (the good life, I know), and I love sourdough bread.
No dairy. I switched to non-dairy instead. Same as gluten, it’s inflammatory for many people.
These changes were mostly based on Dr. Kuon’s advice from her book and the information from the UCSF Long COVID clinic (I shared that last time). In her book, Dr. Kuon provides a lot of detail and scientific background around each of these recommendations. My other sources included the Stanford PACS (Post Acute COVID Syndrome) clinic (which recommends the same anti-inflammatory diet), Michael McCulloch at the Pine Street Clinic (see footnote) and the resources I mentioned in this post - by Dr. Andrew Weil and Dan Neuffer at ANS Rewire.
In case you’re wondering what remains after cutting out so many things - good question. I’m not going to lie, I found it very difficult. My incredible mom and incredible friends were a really big part of making this work. I’ll share some tips next time on what made it a little easier. But mainly I’ll say, depending on your specific body, food intolerances etc, you might not need to be nearly as strict as I was and still see good results - from what I understand, every little shift in the right direction counts. More on that next time, where I’ll write about my mistakes in making these changes.
What I eat today
Since I started feeling better, I’ve also relaxed my restrictions more and more. But, interestingly, I’ve kept a lot of these changes despite feeling better. During recovery, I’ve developed a really finely tuned sense for my body, and now I can often feel a clear & immediate impact from changes to my diet (whereas when I started recovery, I could not tell a difference for months). But I’m certainly not strict about anything anymore - ice cream is back in my life, and it’s glorious :)
Next time, I’ll write about how I made these changes work during recovery, when I had very little energy. I’ll also share some major mistakes I made (like over-doing it, of course), so you can avoid those.
I’m curious - what diet changes have you made during recovery? What’s been working for you? What questions do you have for me? Leave a comment below!
Nicole
University of California, San Francisco
In case you missed the last posts - Dr. Kuon treats patients with chronic fatigue and is Director of the Long COVID OPTIMAL-IH clinic at the University of California, San Francisco
I figured this out with the help of Michael McCulloch, LAc MPH PhD, a fantastic doctor of Traditional Chinese Medicine (TCM) at the Pine Street Clinic (highly recommend if you’re in the Bay Area and looking for holistic care during your recovery). He reviewed my diet and medical history in depth and gave me some good advice during the very depths of my illness. I’ll probably share that experience (my first with TCM) another time.







This is in many ways similar to my own dietary changes made back in 2018.
For any migraine sufferers reading this, the book The Migraine Miracle is a super place to start. Dietary changes simplified - for example, no.1 cut out gluten AND sugar.
Took me months to notice any change to skin, weight, health. And I’d already cut out alcohol and caffeine because I was too ill to drink it.
Reducing inflammation has to be the no.1 priority of those of us living with chronic illness. Diet is huge but there are so many other ways we can reduce inflammation alongside. Eg, the way we speak to ourselves.
For anyone without support be that financial or otherwise, I am someone who didn’t go organic. I didn’t do any of it perfectly. In fact, (miraculously) I put the least amount of pressure on myself to make these type of changes.
In no way am I recommending this as a diet but to give an example of what I ate on the daily:
Porridge oats, with seeds and anti-inflammatory additions like turmeric & cinnamon (even this was regular shop bought milk back then but now I drink raw)
Plate full of raw veg with hummus, cheese, avocado (had this everyday for about 18 months)
Rice dish (often with meat but when I split up
With my boyf my body told me not to buy supermarket meat ever again and I ended up living with a vegetarian for 18 months and it really felt like my body was telling me to detox from meat for a while).
Ladies who menstruate: we need to factor in our menstruation cycle. Alot of information doesn’t factor in our possible need to eat more when around our bleed.
From the off, I allowed myself to “eat what I want, when I want”. The only stipulation was to make it inflammation reducing. So I noticed an increase in the week before my period.
All the info I read said I wouldn’t lose weight this way (didn’t give a shit about weight at that point of illness - my priority as of out of nowhere, became my health).
But the weight did fall off. Massive chunks at a time. With long periods with no weight loss.
People used to ask “what do you eat!?!” But I ate loads of what I could eat and didn’t focus on what I couldn’t.
Food began to taste better. I felt satisfied by what i was eating - for the FIRST time in my life. I put it down to not being super strict that within 12-18 months I realised that this way of eating was sustainable for life. I enjoyed it.
I want readers to know that this is possible. It isn’t about denying, it’s about feeding and fuelling your recovery in a way that work and supports you.
Eventually I became intuitive with my eating. It’s the least recommended option out there but it is possible to tune into your body and what supports you which makes all the conflicting information so much less of an issue (to the point there is no conflict. Your body knows).
Thanks for this post, Nicole. There’s a lot of consistency in what those who have recovered have recommended as far as diet. I went GF and DF for about six months and did not notice any change. I also tried keto, low histamine, no sugar at separate points along the way. I’m working with a nutritionist now and she also helped me see, like you, that I wasn’t getting enough fluids and protein each day. So I’ve made those tweaks. No dramatic changes, but I’m plodding along slowly on my recovery still and have learned to accept that it won’t be a quick process.